Complete Phase 2 Toolkit
This toolkit serves as a communication guide and provides partner resources to help members prepare for renewal. The toolkit and supporting member materials are available in Spanish, Portuguese, Haitian Creole, Vietnamese, Khmer, Chinese, Arabic, and Cape Verdean Creole.
| Language | Download Links |
|---|---|
| English |
MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Spanish |
MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Portuguese (Brazil) | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Haitian Creole | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Vietnamese | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Cape Verdean Creole | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Chinese (Simplified) | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Arabic | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
| Khmer | MassHealth Eligibility Redetermination Outreach Toolkit: Phase 2 |
Introduction and Importance of Communications
In March 2020, the federal government declared a public health emergency (PHE) due to the COVID-19 pandemic. In response to the PHE and consistent with federal requirements, MassHealth put protections in place that prevented members’ MassHealth coverage ending during the COVID-19 emergency.
The federal government ended continuous coverage requirements on April 1, 2023, and MassHealth returned to our regular renewal processes. MassHealth will need to renew all members’ health coverage to ensure they still qualify for their current benefit. These renewals will take place over 12 months, from April 2023 to April 2024. This means that members could get their renewal forms in the mail at any time during this one-year period.
In order to reduce the number of qualified members that lose their coverage, MassHealth is working with the Massachusetts Health Connector, Health Care For All, and other partners to make sure members know how to renew their coverage and know of other affordable health coverage options if needed.
Importance of Communications
Currently, protections are in place that allow all members to keep their MassHealth coverage until April 1, 2023. Beginning April 1, 2023, MassHealth needs to renew all members. These renewals will take place over 12 months. This redetermination process will be the single largest health coverage transition event since the first open enrollment of the Affordable Care Act and the Medicaid expansion. Members need to know what to expect and how to keep their health coverage when MassHealth returns to our regular renewal processes. Most members will either remain eligible for MassHealth or qualify for subsidies that will allow them to get affordable coverage through the Health Connector or other sources.
MassHealth is dedicated to effectively communicating with members and has created cross-agency workgroups to help further develop communications strategies and materials for members who may be hard to reach or have more complex redeterminations, including members experiencing homelessness, members with disabilities, members who are 65 or older, immigrant populations, and children and families.
MassHealth communications have been expanded to include both text and email capabilities. Members who have shared their cell phone number and/or email with MassHealth will receive a text and/or email letting them know their renewal form is coming soon. Renewal forms will be sent to members in a blue envelope.
This toolkit serves as a communications guide and provides resources to support members during their renewals.
The Blue Envelope and Other Important Mail from MassHealth
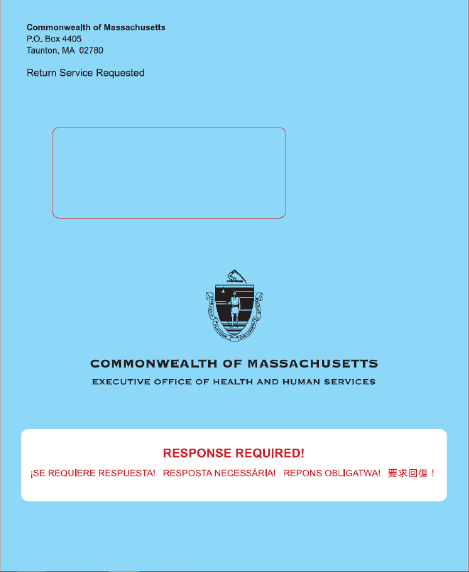
During the redetermination process, MassHealth will be sending out all renewals to members in a blue envelope (pictured below).
A full guide for stakeholders and partners on how to assist a member who has received a blue envelope can be found here.
Inside of each blue envelope members will find the following:
- Their renewal notice, including their renewal deadline,
- An insert about their renewal, and
- A paper renewal form.
Other important mail from MassHealth
During this time period, members may receive other important mail from MassHealth that they must read and respond to in order to maintain their coverage and understand what benefits they qualify for.
This other mail will arrive in white envelopes separately from the Blue Envelope containing the renewal. The return address may indicate “Commonwealth of Massachusetts” or a specific unit of the Commonwealth, such as the Health Insurance Processing Center or EDMC. Members should watch out for any mail that could be from MassHealth, and open all envelopes.
Other important mail may include:
- Requests for Information
- Requests for Verification
- Automatic renewal notices (no action needed)
- Premium bills
- Adult or Child Disability Supplements
- Other documents
Information for Specific Populations
MassHealth has identified five populations that may require dedicated outreach strategies and customized messaging to successfully complete their renewals. These populations require additional outreach because they are hard to reach, have complex renewals, or experience more difficulty completing their renewals. MassHealth has created working groups to better support members at a higher risk of losing coverage, including:
- Older adults (Members aged 65 and older)
- Individuals with disabilities
- Individuals experiencing homelessness
- Individuals who are non-citizens
- Children, families, and pregnant individuals
MassHealth has developed tailored communication materials to reach these populations and the organizations that serve them.
Phase 2 Key and Additional Messages
During Phase 2, MassHealth and its partners should use the following key messages to educate members about the upcoming renewals and make sure they do not have any gaps in coverage.
- Update your information with MassHealth. Make sure MassHealth has your most up to date address, phone number, and email so you do not miss important information and notices from MassHealth.
- Read all your mail. MassHealth will be sending your renewal form in a blue envelope. Additional important notices or request for information may arrive in white envelopes.
- Respond to MassHealth before the deadline. Your notice will have a deadline. Make sure you fill out and send all needed information to MassHealth by the deadline.
Additional Messages:
If you think you might not be eligible for MassHealth, other health coverage options are available.
Massachusetts Health Connector: You may qualify for an affordable plan through the MA Health Connector. Members can visit www.mahealthconnector.org/ or call MA Health Connector at 1-877- MA ENROLL (1-877-623-7773) to learn more or enroll in a plan. If you lose your MassHealth coverage, it is a Qualifying Life Event (QLE). This means you can enroll in a plan through the Health Connector outside of the regular Open Enrollment Period.
Employer Sponsored Insurance: In Massachusetts over 70% of all employers offer health insurance as a benefit to their employees. Most of these employers pay part of the premium and also offer a choice of several health plans. If a member’s employer offers insurance, they can choose the health plan that is best for them from the choices offered. If you have access to an employer-sponsored health plan, your loss of MassHealth coverage is considered a Qualifying Life Event (QLE). The QLE will trigger a Special Enrollment Period (SEP) that will allow you to enroll in your employer’s plan outside of the annual Open Enrollment Period. Generally, the SEP is only available for 60 days following the QLE, so do not wait to review options with your employer.
Medicare Savings Programs: The Medicare Savings Programs (MSP) (formerly known as the MassHealth Senior Buy-In and Buy-In programs) are federally funded programs that pay for some or all of a low-income Medicare recipients’ premiums, deductibles, copayments, and co-insurance.
Prescription Advantage: Prescription Advantage is a state-sponsored prescription drug program for older people and people with disabilities and provides financial help to lower prescription drug costs.
Home and Community Based Waivers, including the Frail Elder Waiver: The Frail Elder Waiver (FEW) is a MassHealth program with expanded income eligibility, administered by the Executive Office of Elder Affairs which provides community supports to Massachusetts residents aged 60 and older who would otherwise require facility care. The FEW supports individuals with a variety of needs that can be met a range of home-based supports.
Program All-inclusive Care for the Elderly: The Program of All-inclusive Care for the Elderly (PACE) is administered by MassHealth and Medicare to provide a wide range of medical, social, recreational, and wellness services to eligible participants. You do not need to be on MassHealth to enroll in PACE.
How to Renew
Once a member receives a blue envelope in the mail, they have a number of ways they can submit their renewal.
To learn more, visit www.mass.gov/how-to/renew-your-masshealth-coverage
“Your Family. Your Health.” Campaign
During Phase 2, MassHealth partnered with the Massachusetts Health Connector and Health Care For All to help educate and notify MassHealth members, focusing on the 15 communities with the highest overall populations of MassHealth members. MassHealth and its partners will execute these outreach efforts in two phases to give individuals and communities information about the renewal process, and to provide local resources to help members successfully complete the renewal process.
The community-oriented campaign will use a three-prong approach to share information and resources with members.
- Door-to-door canvassing: HCFA will hire local canvassers to share materials and resources with individuals and families within the 15 communities to assist them during the redetermination process.
- Sub-grants to community-based organizations (CBOs): CBOs will be awarded funding to conduct education and awareness activities within the communities they serve. Grants will be awarded to CBOs that serve populations in target demographic areas or that serve specific populations, such as members experiencing homelessness or older adults.
- Media buy: Print, digital, radio and television ads will be strategically purchased to help spread awareness of oncoming redeterminations in nine different languages (English, Spanish, Cape Verdean Creole, Portuguese, Haitian Creole, Khmer, Vietnamese, Chinese, and Arabic).
Renewal Resources for Partners and Stakeholders
Partners and stakeholders include any individual or organization who frequently interacts with MassHealth members and has the ability to assist them. This includes staff from community-based organizations, sister agencies, provider organizations, and more.
Partners and stakeholders play a crucial role in helping MassHealth members complete their renewals. There are concrete steps you can take to help MassHealth members through the redeterminations process.
MassHealth has created the following resources to assist these partners and stakeholders:
|
Resource |
Description |
|---|---|
|
A comprehensive resource explaining what you can do as a partner to help MassHealth members, including how to help them prepare for and understand how to complete renewals |
|
|
Redeterminations website: mass.gov/masshealthrenew |
Landing page for redeterminations information, including resources for special populations, videos, and other helpful documents |
In addition to reviewing the MassHealth Renewal Help Guide and other resources, there are other ways that you can help. These include:
1) Signing up for the MassHealth Eligibility Redeterminations Email List. Sign up to receive emails for the latest news and updates on MassHealth’s redetermination process: www.mass.gov/forms/masshealth-eligibility-redeterminations-email-list-sign-up
2) Joining the Massachusetts Health Care Training Forum (MTF) email list and attend trainings. MTF aims to communicate accurate, timely information relating to MassHealth policies and operations, other state programs, and public assistance programs and services to all health care organizations and community-based agencies. Upcoming sessions will focus on MassHealth redeterminations.
Click here to join the email list: www.surveymonkey.com/r/MTFListservNEW2021
For more information, visit the MTF website: www.masshealthmtf.org/
3) Becoming a Certified Application Counselor (CAC). CACs help people apply for health insurance benefits, enroll in health plans, and maintain health insurance coverage. In Massachusetts, the CAC Program is a joint program, administered by MassHealth and supported by the Massachusetts Health Connector.
The CAC Program is a voluntary program; no one pays for the help they receive from a CAC. Individuals do not need a CAC to apply for or receive benefits, but they are an important resource for anyone who has questions about how to apply for health insurance benefits, enroll in health plans, and maintain health insurance coverage. Individuals alone cannot become CACs. Your organization must partner with MassHealth and the Massachusetts Health Connector, and then individuals within your organization can be trained as CACs.
If you are interested in the CAC Program email us at mahealthconnectortraining@massmail.state.ma.us.
Flyers, Posters, and Other Member-Facing Materials
Help us spread the word about MassHealth Redeterminations. Click here to view and download posters, flyers, social media posts, and more! There are general materials and materials targeted to specific populations.
All materials are available in English, Spanish, Portuguese, Haitian Creole, Vietnamese, Khmer, Chinese, Arabic, and Cape Verdean Creole.
Contact for MassHealth Redeterminations Outreach Toolkit
Online
| Date published: | March 24, 2023 |
|---|---|
| Last updated: | March 11, 2024 |