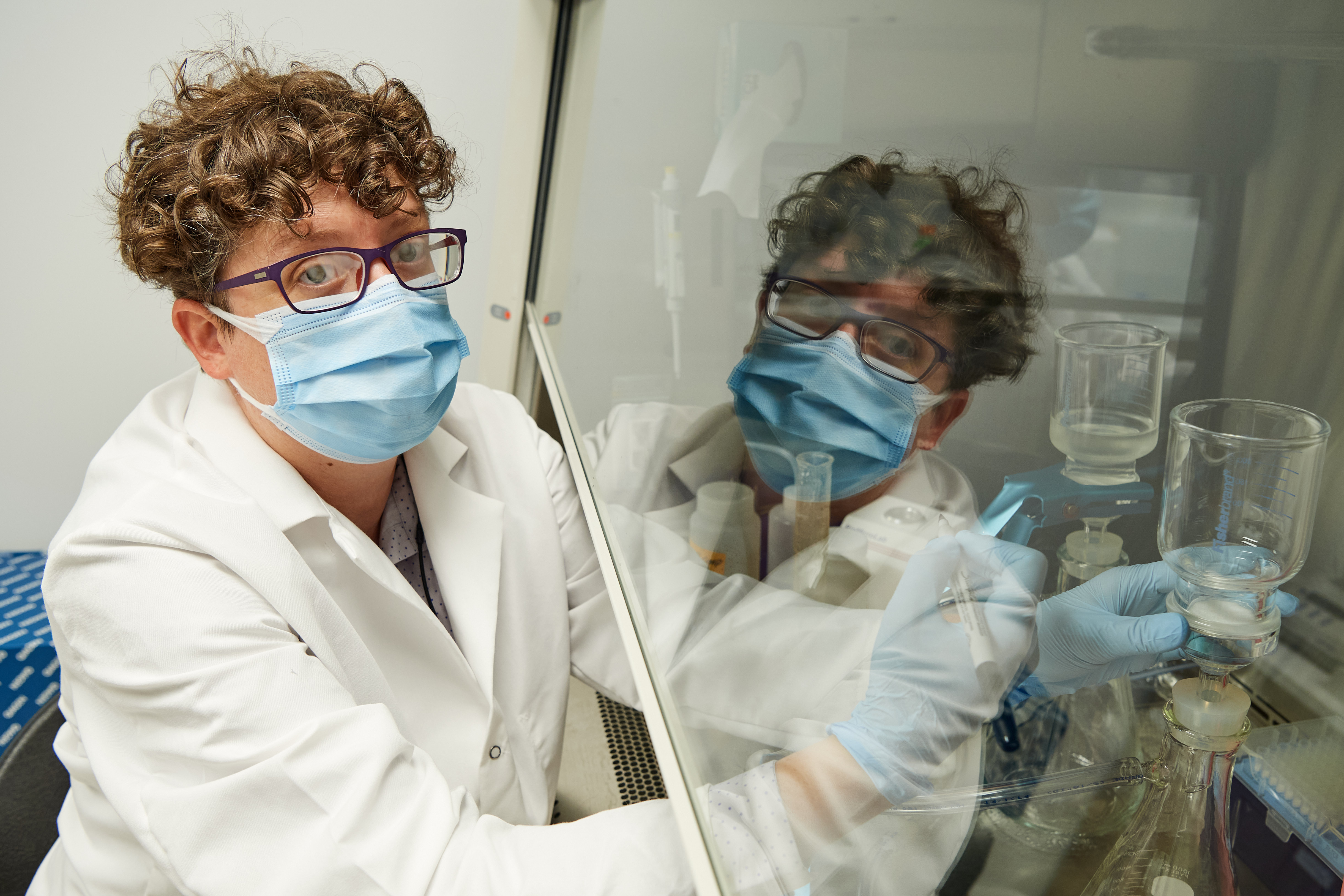
Kendra Maas is a master of the microbiome.
As the facility scientist for UConn’s Microbial Analysis, Resources, and Services laboratory, also known as MARS, she spends a great deal of her time conducting genomic sequencing on bacterial and fungal communities in samples that are brought to her by researchers and that can vary from human or animal specimens to containers of soil taken in field experiments.
“Since I come from a microbiome world, I’m used to dealing with fecal samples or soil samples or these other kinds of samples that are dirtier or more difficult to work with,” says Maas. “And wastewater is really difficult to work with.”
Maas has spent the last several weeks getting better and better at working with wastewater, though, because this fall, she’ll be using skills honed through countless bacterial assays and focusing them on an insidious virus and its presence in wastewater on UConn’s Storrs campus.
“There were several studies pretty early on suggesting that you can measure abundance of COVID-19 genes in wastewater, and that it mirrored the case level – if cases went up, the abundance of COVID that you could measure went up,” says Maas. “What we know now is that it looks like wastewater actually gives you about seven days’ notice – the level of COVID in wastewater goes up seven days before a significant increase in cases gets reported.”
That’s because shortly after an individual contracts the coronavirus, they begin to shed large amounts of the virus through their feces, typically before they show any symptom of illness. Their fecal matter then enters the wastewater system, traveling through a network of sewers and waystations until ultimately, and in the case of a campus like UConn in particular, it ends up at a centralized wastewater treatment facility.
If the source of the COVID in wastewater can be pinpointed where it enters the system, Maas said, this seven-day wastewater warning sign could prove critical in limiting the potential scope of an outbreak on campus.
And that’s exactly what Maas hopes to accomplish as campus reopens for the fall semester and students return to residential living in Storrs.
For weeks, she’s been working out testing methods and protocols to conduct ongoing surveillance of UConn’s wastewater and coordinating with UConn’s Facilities Operations to obtain samples not only from the centralized wastewater treatment plant but also from “lift stations” around campus – pumping stations that help counteract water’s natural downward flow by bringing wastewater from locations at physically lower elevations upward into the system – and potentially other access points.
That’s where UConn’s plan differs from similar wastewater system surveillance already under way in New Haven, for example, where scientists from Yale University are testing for COVID-19 in sludge.
I think one of the duties of UConn being the land grant institution for the state is that we need to be helping the state figure out how to track infection, so that’s my other reason for really wanting to figure out how to do testing as quickly and cheaply as possible in the lab, to be able to open this up to municipalities, or to school districts. — Kendra Maas
“Within the Storrs campus wastewater system, we are able to actually, manually sample from a specific area,” Maas says. “The wastewater treatment plant already collects inlet samples every day, and we can pretty easily put sampling pumps out on the lift stations and collect them.”
Stanley Nolan, UConn’s Director of Utility Operations and Energy Management, says that while they are still evaluating all of the potential access points where sampling pumps could be installed, Facilities Operations sees great value in the wastewater testing protocol.
“Dr. Maas came forward with the potential for testing shortly into the COVID pandemic,” he says, “and being essential employees, and knowing the criticality of this, partnering with student health services and research to do whatever’s necessary to find a solution to this pandemic crisis is an important thing to do. Areas where we have easy access will obviously be tested first. Anything that’s more difficult may require an additional install, and the funding and cost sourcing for that has been provided while the specific locations are still being decided.”
Maas says her ultimate goal is to be able to process these wastewater samples – which must be 24-hour composite samples in order to provide meaningful snapshots of any detectable COVID-19 genetic abundance – and to report back their results within one day.
It’s an ambitious plan for her small lab, which she says will also be assisting Student Health and Wellness with ongoing surveillance testing of students for COVID-19 by providing in-house processing of pooled test samples from student groups.
“Student Health and Wellness is going to be monitoring 5 to 10 percent of the student body, just on a random rolling basis, and MARS will be part of the in-house collaboration of people who are testing pools of samples, likely saliva, for COVID,” she says. “In the meantime, I’ll be testing the wastewater, and if I see a spike in the North Dorms, as an example, then Student Health and Wellness can take their next few days’ worth of random tests and focus them on the North Dorms to try to isolate the individuals.”
Maas and the MARS lab will not know who the individuals who contribute to pooled samples are, she said, but if they detect COVID-19 in those pools, Student Health and Wellness will then be able to contact those individuals for further testing and evaluation by medical professionals.
“The pools will allow us to test a lot more people,” says Maas, and the wastewater can help guide where that pooled testing will be most effectively deployed.
In order to test the wastewater for COVID, though, she first has to concentrate it, which is accomplished by filtering the sample, after which she extracts all of the RNA – COVID-19 and otherwise – that she finds in the filter.
“I expected wastewater to be very gross,” she says. “When you get a half liter of it, it actually isn’t that gross. Especially at UConn in the summer. There aren’t that many people around, so it just looks like kind of cloudy water.”
To see if any of the RNA belongs to the coronavirus, she’s working with two different detection methods – Quantitative Reverse Transcription Polymerase Chain Reaction, or QRT-PCR, the same assay currently used in a vast majority of FDA-approved clinical COVID-19 tests; and Droplet Digital Polymerase Chain Reaction, or DD-PCR, a more sensitive but more time-consuming detection method.
Using these methods, Maas has already found COVID in UConn’s wastewater, even with reduced density as classes went online and large numbers of faculty and staff began telecommuting.
“While I was expecting COVID levels on campus to be very low, I always expected them to be positive,” she says. “When I got the first set of samples in late June, I expected to be able to detect COVID given how high the infection rate was in Connecticut in April and May. I think it’s at pretty low concentrations, and the COVID we’re detecting on campus could be from someone who’s recovered. Or it could also be from someone who’s asymptomatic.”
Because it’s theorized that younger people are more likely to have COVID-19 and remain asymptomatic – yet still able to transmit the virus to others – Maas says wastewater testing could have a significant impact on controlling coronavirus outbreaks on college campuses.
“Unless you’re doing completely random testing and you get lucky, you just won’t find that asymptomatic person,” she says. “And this is a way to catch that – it won’t catch the individual person, but it at least tells us that there are asymptomatic people.”
More broadly, Maas hopes she will be able to continually refine her wastewater COVID-19 detection technique – making it more efficient and cost effective – so that the wastewater surveillance developed at UConn might also be applied to other wastewater systems.
“I think one of the duties of UConn being the land grant institution for the state is that we need to be helping the state figure out how to track infection,” she says, “so that’s my other reason for really wanting to figure out how to do testing as quickly and cheaply as possible in the lab, to be able to open this up to municipalities, or to school districts.”
She continued, “Nobody wants the state of Connecticut to do another blanket shutdown, and this is a way that UConn can help the state potentially avoid another blanket shutdown and instead do targeted shutdowns in select towns or cities throughout the state. If a state shutdown is targeted, maybe we can afford to better support the people in Connecticut who are being directly affected by the shutdown.”
For information about health, safety, and coronavirus testing at UConn in the fall semester, visit reopen.uconn.edu.