Spotlight on a Researcher – Dr. Mark Cayabyab
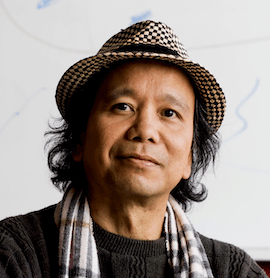
 Mark Cayabyab, Ph.D. is an Associate Professor and Director of Virology and Mucosal Immunology at the College of Dental Medicine at Nova Southeastern University (NSU). He received his Bachelor of Arts degree in Biochemistry, Microbiology, and Immunology at the University of California, Berkeley. He subsequently obtained his Master of Science and PhD in Public Health, Immunology, and Virology at Harvard University studying the role of HIV envelope proteins in the pathogenesis of AIDS. He later conducted his postdoctoral work at Harvard Medical School on HIV Immunology and Vaccinology and was appointed Instructor at the Harvard Dental School. Before joining NSU in 2020, Dr. Cayabyab was an Associate Research Investigator at The Forsyth Institute.
Mark Cayabyab, Ph.D. is an Associate Professor and Director of Virology and Mucosal Immunology at the College of Dental Medicine at Nova Southeastern University (NSU). He received his Bachelor of Arts degree in Biochemistry, Microbiology, and Immunology at the University of California, Berkeley. He subsequently obtained his Master of Science and PhD in Public Health, Immunology, and Virology at Harvard University studying the role of HIV envelope proteins in the pathogenesis of AIDS. He later conducted his postdoctoral work at Harvard Medical School on HIV Immunology and Vaccinology and was appointed Instructor at the Harvard Dental School. Before joining NSU in 2020, Dr. Cayabyab was an Associate Research Investigator at The Forsyth Institute.
Dr. Cayabyab’s research is focused on developing innovative vaccine strategies and therapies against HIV, COVID-19, and other infectious diseases and he possesses over 20 years of research experience in the field HIV/AIDS vaccine development. His research on infectious diseases has resulted in publications in peer-reviewed journals and multiple patents. Currently Dr. Cayabyab’s lab at NSU is focused on exploring novel vaccines and potential therapies to treat HIV and COVID-19 infection.
In a recent publication from the lab, Dr. Cayabyab’s team reported a novel technology for developing an effective vaccine against HIV infection. This can be an important breakthrough in the effort against Acquired Immunodeficiency Syndrome (AIDS) as there are currently no efficient vaccines for this disease. Each year millions of people are infected with Human Immunodeficiency Virus (HIV), and if untreated they suffer from AIDS. Currently, over 1.2 million people in the US and about 38 million people in the world are living with AIDS. In 2019, roughly 690,000 people died from AIDS-related illness and 1.7 million people became newly infected with HIV. Although antiretroviral therapies have been able to slow disease progression or reduce chances of death, to date there is no cure or vaccine for AIDS.
Considering the fatalities and deleterious effects of AIDS all around the world, the development of an effective vaccine is a global health priority. To address this urgent need for efficacious vaccines, researchers at NSU’s College of Dental Medicine, under the leadership of Dr. Cayabyab, attempted to develop immunogens that can be protective against HIV. Their goal was to produce an HIV vaccine that can elicit broadly neutralizing antibodies (bnAbs) or protective antibodies that bind to the HIV envelope glycoprotein variable regions 1 and 2 (V2 apex).
The findings from the research on this novel immunogen related to a possible HIV vaccine were published in 2020 in a peer-reviewed article in the journal AIDS Research and Human Retroviruses. As reported in this publication, Dr. Cayabyab and collaborators proposed a new systematic approach to candidate Env (envelope protein) vaccine selection. The researchers compared side-by-side the structure and antigenicity (ability to be specifically recognized by antibodies generated by immune response) of the three different vaccine candidates for their ability to induce protective antibody responses: BG505 SOSIP.664, 1086.C gp140, and 1086.C gp120. Dr. Cayabyab’s research group used structure, antigenicity, and historical data on their clinical immunogenicity (ability to elicit an immune response) to compare these vaccine candidates. The findings of this study indicate that the BG505 SOSIP.664 trimer and 1086.C gp140 seem to be better vaccine candidates than the monomeric 1086.C gp120, which was recently evaluated to be noneffective in a human HIV vaccine efficacy trial.
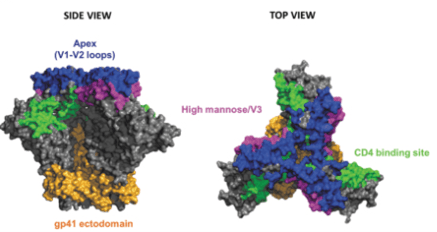
The crystal structure of BG505 SOSIP.664 trimer in a side view (left) and top view (right), and the location of bnAb epitopes: apex, V1-V2 loops (blue), CD4 binding site (green), high mannose patch/V3 (pink), and the gp41 ectodomain (orange).
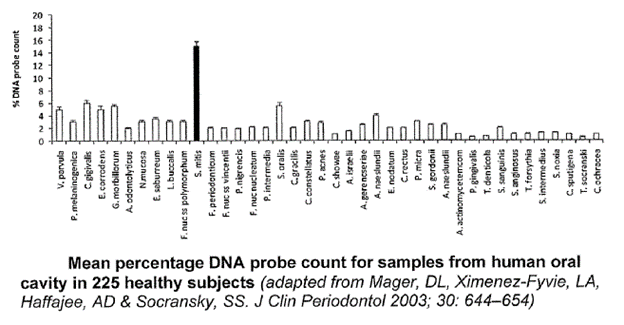
In addition to this work aimed at developing broadly neutralizing antibodies targeting envelope glycoprotein of HIV, Dr. Cayabyab has been developing methods to conduct research and develop other novel strategies for vaccines. His lab has developed a method for eliciting immune response through oral delivery of a Streptococcus mitis (S. mitis) vector. A team of researchers led by Dr. Cayabyab constructed a recombinant S. mitis (rS. mitis) vector that expresses HIV antigens and tested its ability to induce B and T cell responses in the lab in a mouse model. The findings, as published in a peer-reviewed article, indicate that oral inoculation with rS. mitis results in efficient colonization of the oral cavity of mice. Furthermore, this inoculation induced significant systemic and salivary vaccine antigen-specific antibody responses. This novel strategy of applying rS. mitis vaccine vector for the induction of mucosal antibodies can be implemented to prevent penetration of the mucosa by pathogens such as HIV.
As rS. mitis can induce systemic T cell tolerance, its clinical potential is not limited to HIV vaccine. This technology proposed by Dr. Cayabyab has clinical potential for the development of rS. mitis-based therapies for the treatment of various inflammatory, allergic, and autoimmune diseases. Owing to the novelty and translational value of this research, Dr. Cayabyab and his collaborators were granted a patent for this vaccine technology.
Patent: The present invention relates to a new vaccine delivery system.
Research performed by Dr. Cayabyab’s lab for developing novel efficient vaccines has resulted in multiple academic publications. Moreover, this research being conducted at NSU’s College of Dental Medicine has substantial clinical and commercial potential as it offers a solution for major unmet needs in public health. One such vaccine technology developed by Dr. Cayabyab’s lab in NSU has the potential for developing a vaccine that will prevent HIV infection and AIDS. The immunogen developed by Dr. Cayabyab and Dr. Bontempo consists of HIV-1 envelope glycoprotein trimers that can mimic the natural envelope glycoprotein of the HIV-1 virion and can be used to create a vaccine. This immunogen holds significant promise as a possible vaccine candidate against HIV infection.
Considering the translational value of this innovation, NSU’s Office of Technology Transfer worked extensively with Dr. Cayabyab to file a patent application for this invention and now this vaccine technology is available for licensing and further commercialization.
Dr. Cayabyab’s research in the field of HIV, COVID-19, and other infectious diseases holds immense clinical potential. His dedication to innovation in the field of vaccine development ensures that he will continue to make important scientific discoveries at NSU and make a positive impact towards improving prevention and treatment of infectious diseases.