Michigan Maternal Mortality Surveillance Report
Causes and numbers of maternal mortality.By MORGAN WOMACK
Capital News Service
LANSING — When women on psychiatric medication get pregnant, some providers advise them to stop medication to avoid potential risk to the fetus.
But that can be fatal.
Eighty to 90 women die annually in the state during their pregnancy or first year after giving birth, Michigan Maternal Mortality Surveillance Program records show.
And a new study found a majority of maternal suicide or overdose deaths are due to lack of behavioral health care.
“We need better education across the board to all providers that just because a woman gets pregnant, doesn’t mean you have to stop all of her medications,” obstetrician-gynecologist Renee Sundstrom of Central Michigan University (CMU) said.
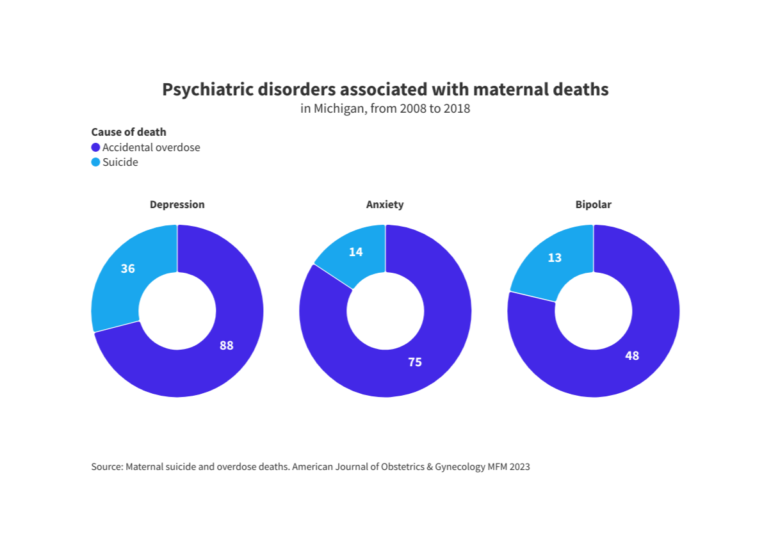
The study, by researchers at Wayne State University, University of Michigan and Duke University, found there were 237 maternal deaths due to suicide or overdoses between 2008 and 2018. Of these women, 70.9% had documented psychiatric illnesses.
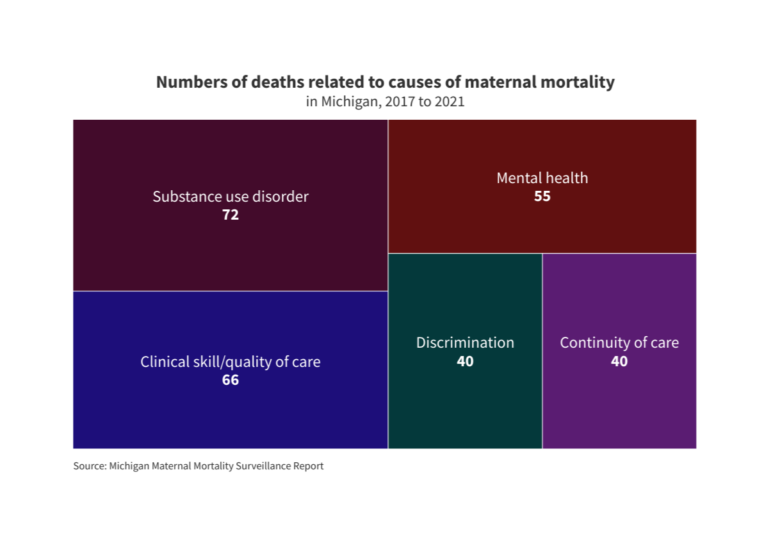
The latest report from the Maternal Mortality Surveillance Program, run by the state Department of Health and Human Services, covers deaths from 2017 to 2021 and makes recommendations to health care providers based on its findings.
The report said that mental health was a factor in 42.6% of the maternal deaths, and substance use disorder was a factor in 55.8%.
Dawn Shanafelt, the director of the Division of Maternal and Infant Health in Health and Human Services, listed 211 — a hotline to help with health and human services needs — and MC3 Perinatal — a psychiatry support program for providers — as important resources for Michigan to promote.
In the report, the surveillance team issued recommendations for the Michigan Perinatal Quality Collaborative — composed of health care leaders and health department professionals
One recommendation was full implementation of what are called ‘safety bundles’: Online resources for providers with information and advice to improve patient safety. The team also called for more statewide education about pregnancy and more partnerships between providers and support services.
Sundstrom, the OB/GYN residency director at CMU Health/ CMU Medical Education Partners, said one solution is medication-assisted care. She said obstetricians and maternal-fetal medicine specialists can determine the risk of taking medications to help pregnant women make a decision.
In 1979, the Food and Drug Administration put medications in different letter categories – A through D and X – depending on their risk to a fetus. While this categorization has since been updated, Sundstrom said some providers still use the system.
Some category B and C drugs include basic painkillers like acetaminophen and various antibiotics, antidepressants, diuretics and anticonvulsants.
Sundstrom said providers shy away from allowing mothers-to-be to take medications in the B or C category, but that most of the medications her hospital uses in pregnancy care are in the B and C categories.
She said providers should learn more information before cutting out such medications for their patients.
According to the study by Wayne State, U-M and Duke, only 27.4% of the women who died due to overdose and suicide during pregnancy or after giving birth received medication-assisted treatment.
Another challenge, Sundstrom said, is that there are not many psychiatric facilities in Michigan that accept pregnant patients.
“We do need to have a multidisciplinary approach to these patients who are at risk,” Sundstrom said. “We need to make sure they have the support they need from their OB provider, from their psychiatric or psychological care provider, even prescribing medication-assisted treatment.”
She said initiatives like CenteringPregnancy, where women with similar due dates meet to talk throughout their pregnancy, can be helpful for learning about different prenatal care practices. CenteringPregnancy is a type of prenatal care offered to patients through Michigan Medicine, the University of Michigan-based hospital system.
“Educating the patient empowers them to take control of their own health and their own well-being, and potentially advocate for themselves a little better than they do or think that they can,” Sundstrom said.
Editor’s note: This story was updated March 29 to clarify Renee Sundstrom’s title.
American Journal of Obstetrics and Gynecology
Psychiatric disorders associated with maternal deaths