Abstract
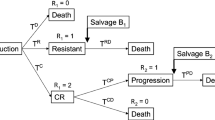
In this work, we demonstrate a mathematical technique for optimizing combination regimens with constraints. We apply the technique to a mathematical model for treatment of patients with chronic myeloid leukemia. The in-host model includes leukemic cell and immune system dynamics during treatment with tyrosine kinase inhibitors and immunomodulatory compounds. The model is minimal (semi-mechanistic) with just enough detail that all relevant therapeutic effects can be represented. The regimens are optimized to yield the highest possible reduction in disease burden, taking into account dosing constraints and side effect risks due to drug exposure. We compare the following three types of regimens: (1) regimens that are restricted to certain discrete dose levels, which can only change every three months; (2) optimal regimens determined using optimal control; and (3) regimens that are piecewise-constant like the first type of regimen, but are obtained as approximations to the optimal control regimens. All three types of regimens result in similar outcomes, but the last one is easy to compute in addition to being clinically feasible.





Similar content being viewed by others
References
Afenya EK, Calderón C (2000) Diverse ideas on the growth kinetics of disseminated cancer cells. Bull Math Biol 62(3):527–542
Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J, Cervantes F, Deininger M, Gratwohl A, Guilhot F, Hochhaus A, Horowitz M, Hughes T, Kantarjian H, Larson R, Radich J, Simonsson B, Silver RT, Goldman J, Hehlmann R (2009) Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol 27:6041–6051
Barbarossa MV, Kuttler C, Zinsl J (2012) Delay equations modeling the effects of phase-specific drugs and immunotherapy on proliferating tumor cells. Math Biosci Eng 9(2):241–257
Barish S, Ochs MF, Sontag ED, Gevertz JL (2017) Evaluating optimal therapy robustness by virtual expansion of a sample population, with a case study in cancer immunotherapy. PNAS 114(31):E6277–E6286. https://doi.org/10.1073/pnas.1703355114
Bonnard B, Chyba M (2003) Singular trajectories and their role in control theory. Mathématiques & Applications, vol 40. Springer, Paris
Bressan A, Piccoli B (2007) Introduction to the mathematical theory of control. American Institute of Mathematical Sciences (AIMS), Providence
Bristol-Myers Squibb (2000) A phase 1B study to investigate the safety and preliminary efficacy for the combination of dasatinib plus nivolumab in patients with chronic myeloid leukemia. In: ClinicalTrials.gov [Internet]. National Library of Medicine (US), Bethesda, MD. [cited 2016 Mar 7]. http://clinicaltrials.gov/show/NCT02011945
Castiglione F, Piccoli B (2006) Optimal control in a model of dendritic cell transfection cancer immunotherapy. Bull Math Biol 68(2):255–274
Chereda B, Melo JV (2015) Natural course and biology of CML. Ann Hematol 94(Suppl 2):S107–S121
Dasatinib (2006) [package insert] Bristol-Myers Squibb Company, Princeton. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021986s7s8lbl.pdf
de Pillis LG, Gu W, Radunskaya AE (2006) Mixed immunotherapy and chemotherapy of tumors: modeling, applications and biological interpretations. J Theor Biol 238(4):841–862
de Pillis LG, Eladdadi A, Radunskaya AE (2014) Modeling cancer-immune responses to therapy. J Pharmacokinet Pharmacodyn 41:461–478
Deininger M, O’Brien SG, Guilhot F, Goldman JM, Hochhaus A, Hughes TP, Radich JP, Hatfield AK, Mone M, Filian J, Reynolds J, Gathmann I, Larson RA, Druker BJ (2009) International randomized study of interferon vs STI571 (IRIS) 8-year follow up. ASH Annu Meet Abstr 22:1126
d’Onofrio A (2005) A general framework for modeling tumor-immune system competition and immunotherapy: Mathematical analysis and biomedical inferences. Physica D Nonlinear Phenom 208:220–235
Dulucq S, Mahon F-X (2016) Deep molecular responses for treatment-free remission in chronic myeloid leukemia. Cancer Med. https://doi.org/10.1002/cam4.801
Faderl S, Talpaz M, Estrov Z, O’Brien S, Kurzrock R, Kantarjian H (1999) The biology of chronic myeloid leukemia. N Engl J Med 341(3):164–172
Farkona S, Diamandis D, Blasutig I (2016) Cancer immunotherapy: the beginning of the end of cancer? BMC Med 14:73
Fokas AS, Keller JB, Clarkson BD (1999) Mathematical model of granulocytopoesis and chronic myelogeneous leukemia. Cancer Res 51:2084–2091
Imatinib (2001) [package insert] Novartis Pharma Stein AG, Stein. https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021588s024lbl.pdf
Ishida Y, Murai K, Yamaguchi K, Miyagishima T, Shindo M, Ogawa K, Nagashima T, Sato S, Watanabe R, Yamamoto S, Hirose T, Saitou S, Yonezumi M, Kondo T, Kato Y, Mochizuki N, Ohno K, Kishino S, Kubo K, Oyake T, Ito S, the Inter-Michinoku Dasatinib Study Group (IMIDAS) (2016) Pharmacokinetics and pharmacodynamics of dastinib in the chronic phase of newly diagnosed chronic myeloid leukemia. Eur J Pharmacol 72:185–193
Kirschner D, Panetta JC (1998) Modeling immunotherapy of the tumor-immune interaction. J Math Biol 37:235–252
Komarova NL (2011) Mathematical modeling of cyclic treatments of chronic myeloid leukemia. Math Biosci Eng 8(2):289–306
Kreutzman A, Juvonen V, Kairisto V, Ekblom M, Stenke L, Seggewiss R, Porkka K, Mustjoki S (2010) Mono/oligoclonal T and NK cells are common in chronic myeloid leukemia patients at diagnosis and expand during dasatinib therapy. Blood 116(5):771–782
Kreutzman A, Porkka K, Mustjoki S (2013) Immunomodulatory effects of tyrosine kinase inhibitors. Int Trends Immunol 1:17–28
Kreutzman A, Ilander M, Porkka K, Vakkila J, Mustjoki S (2014) Dasatinib promotes Th1-type responses in granzyme B expressing T-cells. Oncoimmunology 29(3):e28925
Kronik N, Kogan Y, Elishmereni M, Halevi-Tobias K, Vuk-Pavlović S, Agur Z (2010) Predicting outcomes of prostate cancer immunotherapy by personalized mathematical models. PLoS ONE 5(10):1–8
Ledzewicz U, Moore H (2016) Dynamical systems properties of a mathematical model for treatment of CML. Appl Sci 6:291. https://doi.org/10.3390/app6100291
Ledzewicz U, Moore H (2018) Optimal control applied to a generalized Michaelis-Menten model of CML therapy. Discrete Contin Dyn Syst Ser B 23(1):331–346
Ledzewicz U, Faraji Mosalman MS, Schättler H (2013) Optimal controls for a mathematical model of tumor-immune interactions under targeted chemotherapy with immune boost. Discrete Contin Dyn Syst Ser B 18:1031–1051. https://doi.org/10.3934/dcdsb.2013.18.1031
Machado MP, Tomaz JP, Lorand-Metze I, de Souza CA, Vigorito AC, Delamain MT, Bendit I, Pereira NF, Barbosa Pagnano KB (2011) Monitoring of BCR-ABL levels in chronic myeloid leukemia patients treated with imatinib in the chronic phase - the importance of a major molecular response. Rev Bras Hematol Hemoter 33(3):211–215. https://doi.org/10.5581/1516-8484.20110056
Mahon F-X, Réa D, Guilhot J, Guilhot F, Huguet F, Nicolini F, Legros L, Charbonnier A, Guerci A, Varet B, Etienne G, Reiffers J, Rousselot P, on behalf of the Intergroupe Français des Leucémies Myéloïdes Chroniques (FILMC) (2010) Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol 11(11): 1029–1035
Moore H, Li NK (2004) A mathematical model for chronic myelogenous leukemia (CML) and T cell interaction. J Theor Biol 227:513–523
Moore H, Strauss L, Ledzewicz U (2015) Mathematical optimization of combination therapy for chronic myeloid leukemia (CML). A poster presented at the 6th American conference on pharmacometrics (ACoP), Crystal City, VA, 4–7 October
Nakamura-Ishizu A, Takizawa H, Suda T (2014) The analysis, roles and regulation of quiescence in hematopoietic stem cells. Development 141:4656–4666
Nanda S, Moore H, Lenhart S (2007) Optimal control of treatment in a mathematical model of chronic myelogenous leukemia. Math Biosci 210:143–156
Nivolumab (2014) [package insert] Bristol-Myers Squibb Company, Princeton. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/125554lbl.pdf
Pardoll DM (2012) The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 12(4):252–264
Pontryagin LS, Boltyanskii VG, Gamkrelidze RV, Mishchenko EF (1964) The mathematical theory of optimal processes. MacMillan, New York
Press RD, Love Z, Tronnes AA, Yang R, Tran T, Mongoue-Tchokote S, Mori M, Mauro MJ, Deininger MW, Druker BJ (2006) BCR-ABL mRNA levels at and after the time of a complete cytogenetic response (CCR) predict the duration of CCR in imatinib mesylate-treated patients with CML. Blood 107:4250–4256. https://doi.org/10.1182/blood-2005-11-4406
Prinz H (2010) Hill coefficients, dose-response curves and allosteric mechanisms. J Chem Biol 3(1):37–44
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, Dang P, Goyne JM, Slader C, Filshie RJ, Mills AK, Melo JV, White DL, Grigg AP, Hughes TP (2013) Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 122(4):515–522
Rubinow SI (1969) A simple model of steady state differentiating cell system. J Cell Biol 43:32–39
Rubinow SI, Lebowitz JL (1975) A mathematical model of neutrophil production and control in normal men. J Math Biol 1:187–225
Sawyers CL (1999) Chronic myeloid leukemia. N Engl J Med 340(17):1330–1340
Schättler H, Ledzewicz U (2012) Geometric optimal control. Springer, New York
Schättler H, Ledzewicz U (2015) Optimal control for mathematical models of cancer therapies. Springer, New York
Serre R, Benzekry S, Padovani L, Meille C, André N, Ciccolini J, Barlesi F, Muracciole X, Barbolosi D (2016) Mathematical modeling of cancer immunotherapy and its synergy with radiotherapy. Cancer Res 76(17):4931–4940
Shahriyari L, Komarova NL (2013) Symmetric vs. asymmetric stem cell divisions: an adaptation against cancer? PLoS ONE 8(10):e76195. https://doi.org/10.1371/journal.pone.0076195
Shudo E, Ribeiro RM, Perelson AS (2009) Modelling hepatitis C virus kinetics: the relationship between the infected cell loss rate and the final slope of viral decay. Antiviral Therapy 14(3):459–64
Stengel RF, Ghigliazza R, Kulkarni N, Laplace O (2002) Optimal control of innate immune response. Optim Control Appl Methods 23:91–104
Talpaz M, Kantarjian H, McCredie K, Trujillo J, Keating M, Gutterman JU (1987) Therapy of chronic myelogenous leukemia. Cancer 59:664–667
Weiden PL, Sullivan KM, Flournoy N, Storb R, Thomas ED, Seattle Marrow Transplant Team (1981) Antileukemic effect of chronic graft-versus-host disease: contribution to improved survival after allogeneic marrow transplantation. N Engl J Med 304:1529–1533
Weinberg RA (2007) The biology of cancer. Taylor & Francis, New York
Wilson S, Levy D (2012) A mathematical model of the enhancement of tumor vaccine efficacy by immunotherapy. Bull Math Biol 74(7):1–20
Acknowledgements
The first and second author were employed by and own stock in Bristol-Myers Squibb. The third author received financial support from Bristol-Myers Squibb during this project.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 Optimal constrained solutions with generalized Hill coefficients in the dynamics
In the model dynamics (1)–(3), we have used Michaelis-Menten terms to represent the drug effects; we have also have used analogous expressions to model some of the interactions between populations. More generally, the drug effects could be represented by a sigmoidal relationship of the form
with a Hill coefficient \(n \ge 1\) (Prinz 2010). In principle, the coefficient n could be drug-dependent and could even depend on which particular drug interaction is being modeled leading to a large variety of situations. Here we give some optimal solutions using the same exponent n in each of the drug-related terms and also for the interaction terms among the populations. Figures 6, 7 and 8 show the optimal year-long constrained solutions for Hill coefficients \(n=1.5\), \(n=2\) and \(n=2.7\) iterated over five years. We chose the value \(n=2.7\) based on data for dasatinib (approximate mean \(IC_{50}\) and \(IC_{90}\) concentrations of CD34+ cells) in the paper by Ishida et al. (2016). The range of \(IC_{50}\) values feasible for these data is large and skewed right (from 0.41 to 50 ng/mL with a median of 4.3). If we assume that a representative \(IC_{50}\) value is 6.5, and plug in an \(IC_{90}\) value of 14.3 for u in Eq. (5), we can numerically determine that \(n = 2.7\) makes the expression in Eq. (5) close to 0.9, as desired (that is, the expression gives \(90\%\) when we plug in an \(IC_{90}\) value for u). The weights in the objective are the same ones that were used before (see the section Constrained Optimization of CML Therapy).
\((\hbox {n} = 1.5)\) Solutions for the constrained optimization problem [Opt] with piecewise-constant controls in the class \(\mathcal {U}_{pc}\), iterated year by year. The graphs show the solutions for years 1 (top), 3 (middle), and 5 (bottom). The dose levels are shown on the left and the resulting populations on the right. A Hill coefficient of \(\mathbf {n=1.5}\) was used in the dynamics to describe all pharmacodynamic relations in Eqs. (1)–(3) in the form \(\frac{u^n}{UC_{50}^n+u^n}\)
\((\hbox {n} = 2)\) Solutions for the constrained optimization problem [Opt] with piecewise-constant controls in the class \(\mathcal {U}_{pc}\), iterated year by year. The graphs show the solutions for years 1 (top), 3 (middle), and 5 (bottom). The dose levels are shown on the left and the resulting populations on the right. A Hill coefficient of \(\mathbf {n=2}\) was used in the dynamics to describe all pharmacodynamic relations in Eqs. (1)–(3) in the form \(\frac{u^n}{UC_{50}^n+u^n}\)
\((\hbox {n} = 2.7)\) Solutions for the constrained optimization problem [Opt] with piecewise-constant controls in the class \(\mathcal {U}_{pc}\), iterated year by year. The graphs show the solutions for years 1 (top), 3 (middle), and 5 (bottom). The dose levels are shown on the left and the resulting populations on the right. A Hill coefficient of \(\mathbf {n=2.7}\) was used in the dynamics to describe all pharmacodynamic relations in Eqs. (1)–(3) in the form \(\frac{u^n}{UC_{50}^n+u^n}\)
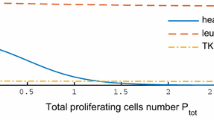
The graphs in Figs. 6, 7, and 8 show the changes in the optimal constrained controls for various values of the exponent n. In the first year, all controls are at full dose irrespective of the exponent, but as the values for P decrease, changes in the controls \(u_1\) and \(u_2\) arise. Generally, the doses for \(u_1\) and \(u_2\) are lower in subsequent years and on similar levels as for the case \(n=1\) shown in Fig. 2, but the timing of the switching varies. The use of lower doses towards the end of the year and the associated increase in tumor volume then leads to higher doses at the beginning of the subsequent years. The control \(u_3\) generally is at full dose throughout all five years, and only for \(n=2.7\) does the dose drop, with \(u_3=0\) in the last quarter of year 5. Table 3 lists the cell population values of the states after years 1, 3, and 5. Overall, for these scenarios the Michaelis-Menten functional relation with \(n=1\) corresponds to a conservative estimate for the effectiveness of therapy as far as the terminal values for the states Q and E are concerned. The final values for P depend more on the overall amounts of drugs used and here there is no clear relation with the exponent n. This mostly is caused by the fact that the effects of one year’s regimen propagate to the next year which almost leads to periodic behavior: if the initial tumor volumes are low, low drug doses are administered, which allows P to increase, which then leads to the administration of higher doses and lowering of P in the following year.
1.2 Optimal solutions for different weights \(\gamma _i\) in the objective functional
The choice of weights in the objective is an essential aspect of the optimization and generally one does not know the “correct” values to use. Although data are available on the severity of adverse events for the three classes of therapies included in this work (Imatinib 2001, Dasatinib 2006, Nivolumab 2014), and one can form an opinion of a relative ranking for the three compounds, we do not make any such claims in this work. We simply include hypothetical illustrations for how optimal solutions react to different assessments of the side effects of the drugs. We explore the structure of optimal solutions for another example here, setting
In this case, we have assigned a higher toxicity penalty to \(u_2\) than \(u_1\), and we have increased the toxicity penalty for \(u_3\). Otherwise, the same initial conditions, dose level limits and parameters as before were used. Figure 9 compares unconstrained optimal controls with optimal constrained regimens in \(\mathcal{U}_{pc}\). With these weights, the disease burden in year 1 is still so high that full-dose therapies are optimal. However, once the values of P decrease, because of the higher weights on the controls (i.e., assumed-higher side effects), the optimal dose levels decrease more than in the case considered previously. The dose levels for \(u_3\) are now so small that they are all approximated with 0. Indeed, the optimal solutions in the class \(\mathcal{U}_{pc}\) often take the value zero during the last quarter of the later years.
Comparison of the unconstrained optimal control solutions in \(\mathcal{U}\) (left) with constrained optimal regimens in \(\mathcal{U}_{pc}\) for years 1, 3, and 5 (top to bottom) and weights \(\gamma _1 = \frac{3}{u_1^{\max }}\), \(\gamma _2 = \frac{5}{u_2^{\max }}\) and \(\gamma _3 =\frac{3}{u_3^{\max }}\)
We also include several examples for a five-year treatment period. As before, the weights \(\gamma _i\) are scaled with their maximum values in the form \(\gamma _i = \tilde{\gamma }_i/u_i^{\max }\) for \(i = 1, 2, 3\). We have fixed \(\tilde{\gamma }_3=20\), but have used different weights on the controls \(u_1\) and \(u_2\) to give one or the other a higher weight for toxicity. The numerical values of the weights for our runs are given in Table 4. In runs A and B, shown as the top and middle rows of Fig. 10, respectively, the left-hand column shows control \(u_1\) with a higher assigned toxicity than \(u_2\), with the highest weight on \(u_1\) in run A. The optimal controls and their piecewise-constant approximations incorporate these adjustments in the weights and result in lower drug dose levels.
Optimal controls in \(\mathcal{U}\) (left) and the resulting populations (right) over a five-year treatment period with different weights \(\tilde{\gamma }\): \(\tilde{\gamma }_1=250\) and \(\tilde{\gamma }_2=100\) for run A (top row), \(\tilde{\gamma }_1=150\) and \(\tilde{\gamma }_2=50\) for run B (middle row), and \(\tilde{\gamma }_1=50\) and \(\tilde{\gamma }_2=250\) for run C (bottom row). The weight \(\tilde{\gamma }_3\) is fixed to 20 for all of these runs
Optimal controls in \(\mathcal{U}\) (left) and the resulting cell populations (right) over a three-month treatment period with MMR. The weights used are: (top) \(\tilde{\gamma }_1=10\), \(\tilde{\gamma }_2=3\), and \(\tilde{\gamma }_3=1\); and (bottom) \(\tilde{\gamma }_1=25\), \(\tilde{\gamma }_2=40\), and \(\tilde{\gamma }_3=3\)
1.3 Maintenance programs and elimination therapies
Model parameters are patient-specific and responses range from long-term survival to almost no effect from the therapy. So far we have considered situations that lie in between these two extremes. Our numerical examples illustrate scenarios that correspond to what could be considered management of the disease over a longer treatment period in a maintenance program. In this section, we include examples in which almost complete eradication of the disease is reached within a short period. Specifically, we include examples in which a reduction of the original BCR-ABL1 levels to less than \(0.1 \%\) of the original disease burden [known as major molecular response, or MMR (Baccarani et al. 2009)] is accomplished in a three-month period. Such behavior is only seen for certain sets of parameter values. The parameter values shown in Table 5 were used in the dynamics for the numerical examples in this section. Parameters that are not listed in Table 5 are the same as in Table 1 in the paper.
We used the following weights in the objective:
We used various weights in the objective for the toxicity on the controls \(u_1\), \(u_2\), and \(u_3\). In the run shown in the top row of Fig. 11 we used \(\tilde{\gamma }_1=10\), \(\tilde{\gamma }_2=3\), and \(\tilde{\gamma }_3=1\). For these weights, the drugs \(u_2\) and \(u_3\) end up at full dose levels throughout the three-month therapy interval . The drug assigned a higher toxicity penalty (in this case, \(u_1\)) starts at full dose, but very quickly is reduced to lower dose levels. The values for the leukemic populations after three months are given by \(P(3)=0.895\) and \(Q(3)=0.028\). This reflects a reduction of P to less than \(0.1 \%\) of its initial value (MMR) and a large reduction in the value of Q, as well. In the second run, shown in the bottom row of Fig. 11, the control \(u_2\) is assigned a higher toxicity penalty. The weights used are \(\tilde{\gamma }_1=25\), \(\tilde{\gamma }_2=40\), and \(\tilde{\gamma }_3=3\). Although \(u_2\) is assigned higher toxicity in this run, overall it is the more effective TKI drug in our model and thus it is only reduced towards the end of therapy. Control \(u_1\) follows the same pattern as in the other run, since its assigned toxicity penalty is still quite high. As a result, the leukemic cell reductions are smaller and now the values are \(P(3)=1.950\) and \(Q(3)=0.029\). The higher P level illustrates the role of the second drug \(u_2\) in reducing the leukemic cell populations in our model.
1.4 Summary
In this work, we have computed optimal regimens for combination therapy of CML patients, with constraints on dose levels and the times when they can be changed. Using optimal control, we also computed regimens that are optimal and allowed to change continuously at any time. A comparison showed that the two approaches lead to similar outcomes. The first class of solutions, \(\mathcal{U}_{pc}\), is motivated by practical concerns and considers only certain dose levels along with a schedule that only allows the dose to change every three months. The associated optimization problem only has a finite number of choices, but it quickly becomes intractable due to computational complexity. For the second class, \(\mathcal{U}\), only the ranges of the doses have limits, and arbitrary changes are allowed within these limits. So this becomes a finite-dimensional continuous-time optimal control problem (Bonnard and Chyba 2003; Bressan and Piccoli 2007; Pontryagin et al. 1964; Schättler and Ledzewicz 2012), which takes only a few minutes to run. We examined a third class of solutions, obtained by approximating optimal solutions \(u_{*} \in \mathcal{U}\) by functions in \(\mathcal{U}_{pc}\) which are closest to the average of \(u_{*}\) on each quarter year. This third class has the advantage of being tractable, as the optimal control problem is numerically straightforward, as is the calculation of the average values of the controls over three-month intervals. The third class is also clinically feasible, as it only has certain fixed dose levels, which can only change every three months. Examples in this work show that these approximations have almost identical cell population results, which is why the third class of solutions is the one we propose should be used for clinical applications.
Rights and permissions
About this article
Cite this article
Moore, H., Strauss, L. & Ledzewicz, U. Optimization of combination therapy for chronic myeloid leukemia with dosing constraints. J. Math. Biol. 77, 1533–1561 (2018). https://doi.org/10.1007/s00285-018-1262-6
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00285-018-1262-6
Keywords
- Chronic myeloid leukemia (CML)
- Constrained optimization
- Optimal control
- Combination therapy
- Tyrosine kinase inhibitors (TKIs)
- Immunotherapy