Maryland Medicaid Demonstration Project
Of the approximately 1.38 million children and adult beneficiaries enrolled in Maryland’s Medicaid program, approximately 86% are enrolled in the HealthChoice program, Maryland’s statewide mandatory managed care program for Medicaid enrollees. Under HealthChoice, eligible families and individuals are required to enroll in one of nine available managed care organizations (MCO) that have been approved by the Maryland Department of Health (the Department). As of November, 2018, approximately 611,000 adults aged 18-64 were enrolled in HealthChoice MCOs.

A two-year grant award from NACDD beginning in June 2016 allowed Maryland Medicaid, in collaboration with Maryland’s Center for Chronic Disease Prevention and Control (the Center), to design and implement a delivery model for the National Diabetes Prevention Program (National DPP) lifestyle change program to Medicaid enrollees in MCOs. These two agencies are co-located within the Department and both report to the Secretary of Health. Medicaid acted as the fiscal agent for the grant and led grant implementation. The Center offered a statewide focus on building the National DPP, supplied diabetes prevention expertise, and collaborated with Maryland Medicaid to provide technical assistance to MCOs and CDC-recognized organizations who participated in the Demonstration. The Center also maintains a diabetes prevention referral and data collection website, known as behealthymaryland.org.
The organizational structure of Maryland’s Medicaid and National DPP demonstration, as illustrated by the Maryland Department of Health, is in Figure 2. Figure 1 is a similar chart showing how the entities were organized for the purposes of the evaluation (Year 2 only), which required that measurement be at the site of an organization or organizations under one Diabetes Prevention Recognition Program (DPRP) organization code.
Figure 1. Organization of Maryland’s Medicaid Demonstration Project (Year 2)
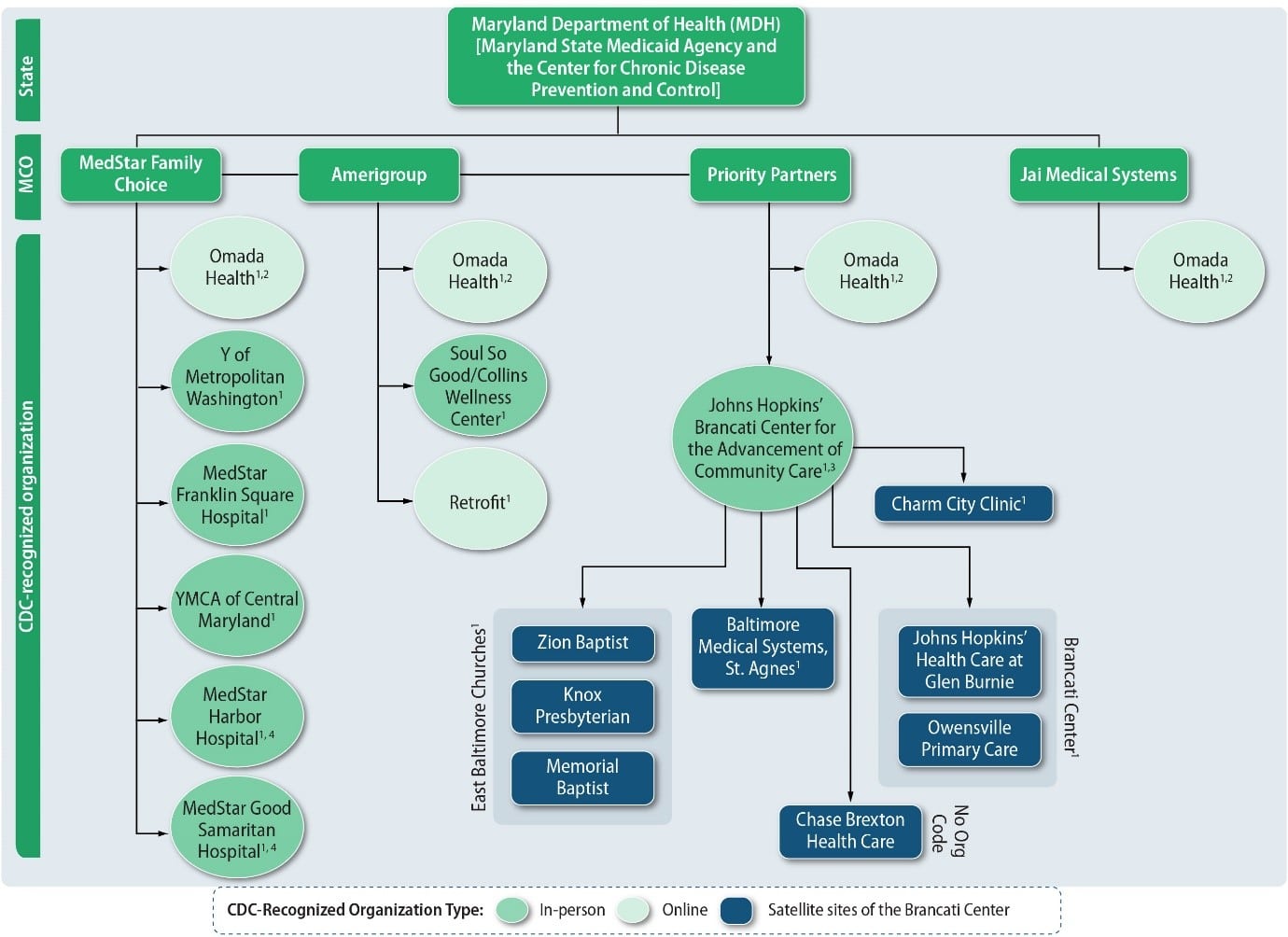
1. Indicates that this entity has a DPRP organizational code.
2. Omada has one DPRP organizational code, even though it works with multiple MCOs and CCOs across states.
3. Under the Johns Hopkins’ Brancati Center for the Advancement of Community Care, Zion Baptist Church, Knox Presbyterian Church, and Memorial Baptist Church are
under one organizational code, “East Baltimore Churches”; Charm City Clinic has its own organizational code; Baltimore Medical System has its own organizational code;
Johns Hopkins Healthcare at Glen Burnie and Owensville Primary Care Center are under one organizational code, “Brancati Center”; and Chase Brexton Health System
does not have an organizational code because it did not apply to CDC’s DPRP, but is still active in the Demonstration. The eight satellite sites structurally appear under
the Brancati Center because although some groups of sites have their own organizational codes, they still operate on behalf of the Center.
4. MedStar Harbor Hospital and MedStar Good Samaritan Hospital did not submit data collection instruments in Year 2, but did enroll participants in Year 2.
Figure 2. Maryland Demonstration Partners
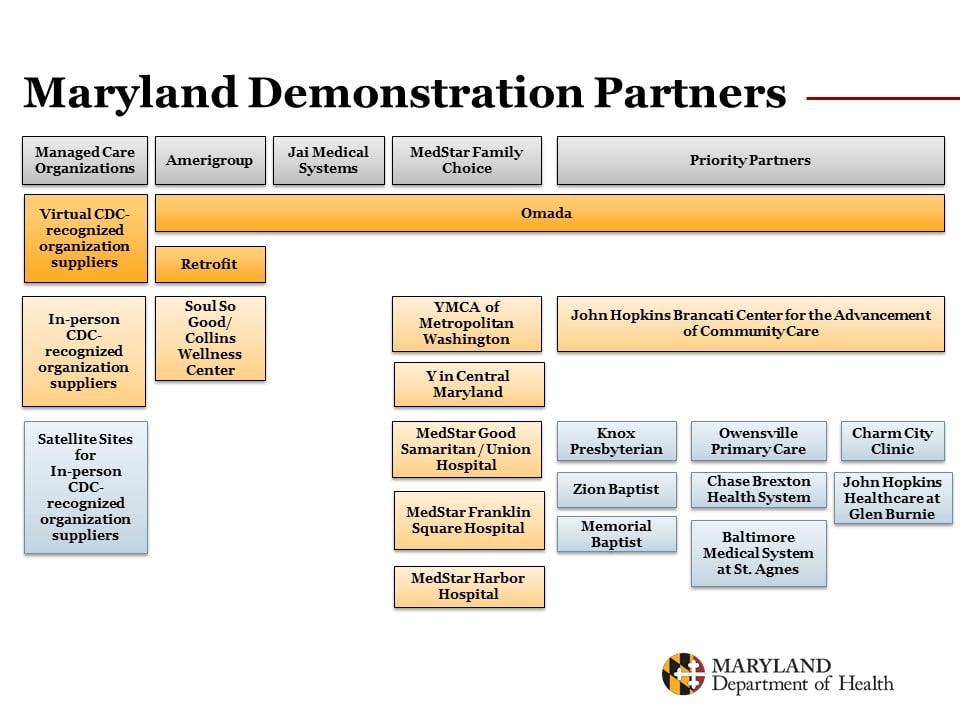
Source: Maryland Department of Health, Sandra Kick, 2018
All eight Medicaid MCOs1 that were participating in HealthChoice in 2016 were invited to participate in the Demonstration; of these, four MCOs—Amerigroup, Priority Partners, Jai Medical Systems, and MedStar Family Choice (MedStar)—agreed to participate and implement the National DPP lifestyle change program to Medicaid beneficiaries at-risk for type 2 diabetes. The intent of the funding was to allow these MCOs to build a sustainable infrastructure for diabetes prevention for their at-risk beneficiaries. Priority Partners, serving approximately 300,248 members in the HealthChoice program, is the largest of the four MCOs, followed by Amerigroup, with approximately 276,558 members; MedStar with approximately 91,376 members; and Jai Medical Systems, with approximately 27,107 members.2
Each of the MCOs contracted with CDC-recognized organizations to provide online or community-based/in-person National DPP lifestyle change programs, or both. All MCOs contracted with Omada Health, an online CDC-recognized organization. Jai Medical Systems utilized Omada Health as their sole CDC-recognized organization, while Amerigroup contracted with a second online CDC-recognized organization, Retrofit, as well as Soul So Good/Collins Wellness Center to provide in-person sessions of the National DPP lifestyle change program. MedStar Family Choice contracted with two YMCAs and two MedStar hospital-run community-based programs to provide the National DPP lifestyle change program in-person. Priority Partners contracted with the Brancati Center for the Advancement of Community Care, a Johns Hopkins School of Medicine entity. The Brancati Center worked closely with Priority Partners to assist in screening of participants and then worked with community-based organizations by providing training, providing materials, managing data and analyses, and providing oversight of programs.
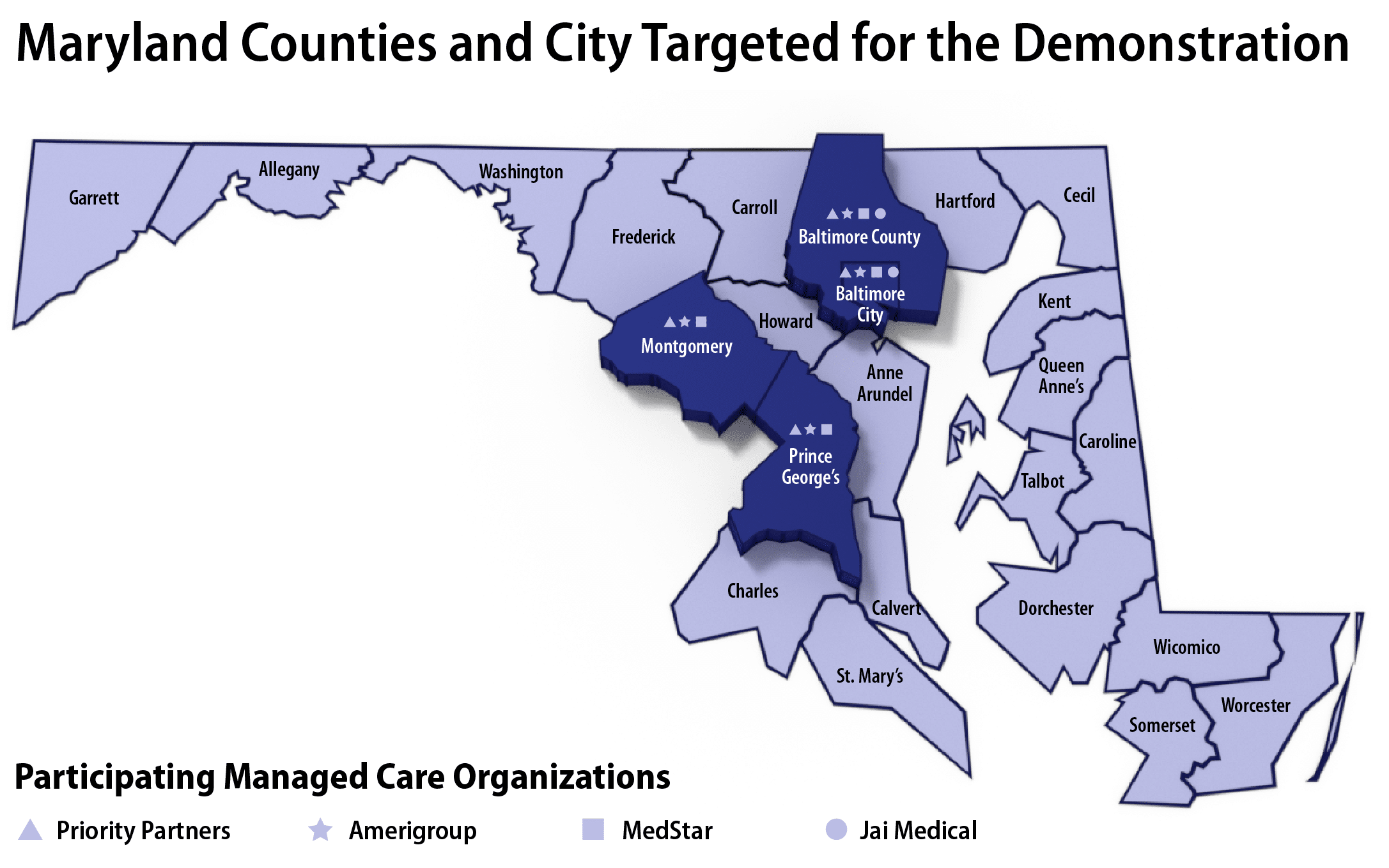
Maryland Medicaid claims data (2013–2015) initially showed that more than 58,000 Medicaid beneficiaries were at risk of developing type 2 diabetes and was later revised after refining the eligibility algorithm used to identify at-risk beneficiaries. Most of these beneficiaries were located in four counties, which Maryland Medicaid targeted in the first year of the Demonstration: Baltimore City, Baltimore County, Montgomery County, and Prince George’s County (as shown in Figure 3). Maryland Medicaid expanded the available jurisdictions statewide during the second year of the Demonstration.
1 Aetna Better Health joined HealthChoice as the ninth MCO in 2018.
2 The Hilltop Institute. (2019, April 30). Maryland Medicaid Management Information System (MMIS) Decision Support System. Retrieved June 7, 2019.
Figure 3. Initial Maryland Counties and City Targeted in the Demonstration (Year 1)
To learn more about outcomes from the Demonstration, please visit the Evaluation page. Maryland created a technical guidance document for their MCOs to successfully implement the National DPP lifestyle change program according to Demonstration guidelines; please find that here. Please note that this document includes guidance for the Medicaid Demonstration Project and certain chapters are no longer current.
Sustainability
In July 2018, Maryland Medicaid successfully applied for an amendment to Maryland’s §1115 HealthChoice demonstration waiver from the Centers for Medicare and Medicaid Services (CMS) to allow continued limited provision of the National DPP lifestyle change program through the four Demonstration MCOs. The final approval, received in March 2019, expanded on this to allow the HealthChoice Diabetes Prevention Program to be implemented statewide, through all nine MCOs, effective July 1, 2019, through December 31, 2021. Then effective January 1, 2022, CMS approved and renewed Maryland’s §1115 demonstration wavier for five years.
A §1115 waiver is one mechanism a state can use to claim federal matching funds for the National DPP lifestyle change program. Maryland chose a §1115 waiver due to the waiver’s flexibility to further test and evaluate the effectiveness of the program on the Medicaid managed care population. To continue to receive federal matching funds after the current waiver expires in 2026, Maryland may apply for a waiver renewal or pursue a state plan amendment (SPA) to the Medicaid State Plan. §1115 waiver renewals are generally granted for an additional three to five years and there is no limit to the number of times the waiver can be renewed. Additional details on Maryland’s §1115 waiver, including the waiver language, can be found on the Attaining Coverage Through a Section 1115 Demonstration Waiver page of the Coverage Toolkit.
To learn more about Maryland’s benefit, please watch the June 15, 2023 NACDD webinar, Maryland and Oregon: Journey from Pilot to Performance, minute 9 through 30 in the recording, and please see the summary resource of the presentation.
New Provider Type for CDC-Recognized Organizations
Maryland Medicaid created a new provider type for CDC-recognized organizations to designate as part of Medicaid’s provider enrollment process and is working on various ways to support and connect CDC-recognized organizations with MCOs to create a robust network of providers to offer the benefit. Maryland’s waiver allows for all CDC approved delivery modes including in-person, online, distance learning, and combination. Maryland began enrolling CDC-recognized organizations into Maryland Medicaid’s electronic Provider Revalidation and Enrollment Portal (ePREP) in May 2019. A summary of how Maryland Medicaid communicated with CDC-recognized organizations about ePREP can be found on the Create a New Provider Type for CDC-Recognized Organizations page of the Coverage Toolkit.
To learn more about Maryland’s HealthChoice Diabetes Prevention Program, please visit Maryland’s HealthChoice Diabetes Prevention Program Information for Providers webpage, which includes many helpful resources such as the HealthChoice Diabetes Prevention Program Manual and a document answering frequently asked questions about program implementation.
Health Information Exchange Engagement
To reduce type 2 diabetes rates, Maryland Medicaid has worked closely with Chesapeake Regional Information System for our Patients (CRISP), the state designated health information exchange (HIE), to identify individuals eligible for participation in the National DPP lifestyle change program and facilitate referrals through a closed-loop electronic referral process.
CRISP uses various data sources to identify individuals with prediabetes who are likely eligible for the National DPP lifestyle change program. CRISP then generates a “Care Alert” for these individuals that communicates eligibility to their health care provider(s). CRISP also uses monthly “SmartAlerts” to alert MCO case management teams of potentially eligible individuals on their rosters. CRISP’s closed-loop (i.e., bi-directional) referral tool (eReferral) allows health care teams to refer eligible individuals to outside organizations offering the National DPP lifestyle change program, and to receive referral status and enrollment updates on the referred individuals.
To learn more about Maryland’s CRISP prediabetes flag and eReferral tool, please see the CRISP one pager. Additional information can be found in the recording and slides from the June 9, 2022 presentation on CRISP at the NACDD General Member Webinar.









